0% Interest For 12 Months On Orders Over $5,000! | Shop Now
0% Interest For 12 Months On Orders Over $5,000! | Shop Now
If there’s one thing I’ve learned over four decades in clinical practice and digital innovation, it’s this: you cannot treat three-dimensional problems with two-dimensional thinking. Every extraction, graft, and implant placement must begin with precise imaging, thoughtful planning, and biologically sound execution. That’s not an opinion – it’s the standard we must uphold if we want to preserve bone, optimize esthetics, and avoid future complications.
Let me walk you through what I believe are the most critical principles for successful socket preservation and grafting and why, in my practice, it’s a non-negotiable option for my patients.
Tooth loss isn’t the end of the story, it’s the beginning of bone loss. The literature shows we can lose up to 40–60% of bone volume within months of extraction, both vertically and horizontally. That kind of resorption doesn’t just affect the future placement of dental implants, it impacts esthetics, function, and patient satisfaction.
So the question isn’t should we graft. The question is why wouldn’t we?
Every time I remove a tooth, I plan to preserve or regenerate bone, even if the patient hasn’t yet committed to an implant. Because when they come back 6 months (or 6 years) later ready for treatment, I want to be able to say: we planned for this. Bone grafting works if done properly with the proper materials and methods.
I’ve been advocating for CBCT since 1985, long before it became standard. Why? Because periapicals lie. A PA can’t show you root morphology, buccal plate thickness, or the angulation of the alveolus. Only 3D imaging combined with treatment planning software provides a complete picture of the patient’s true anatomical presentation.
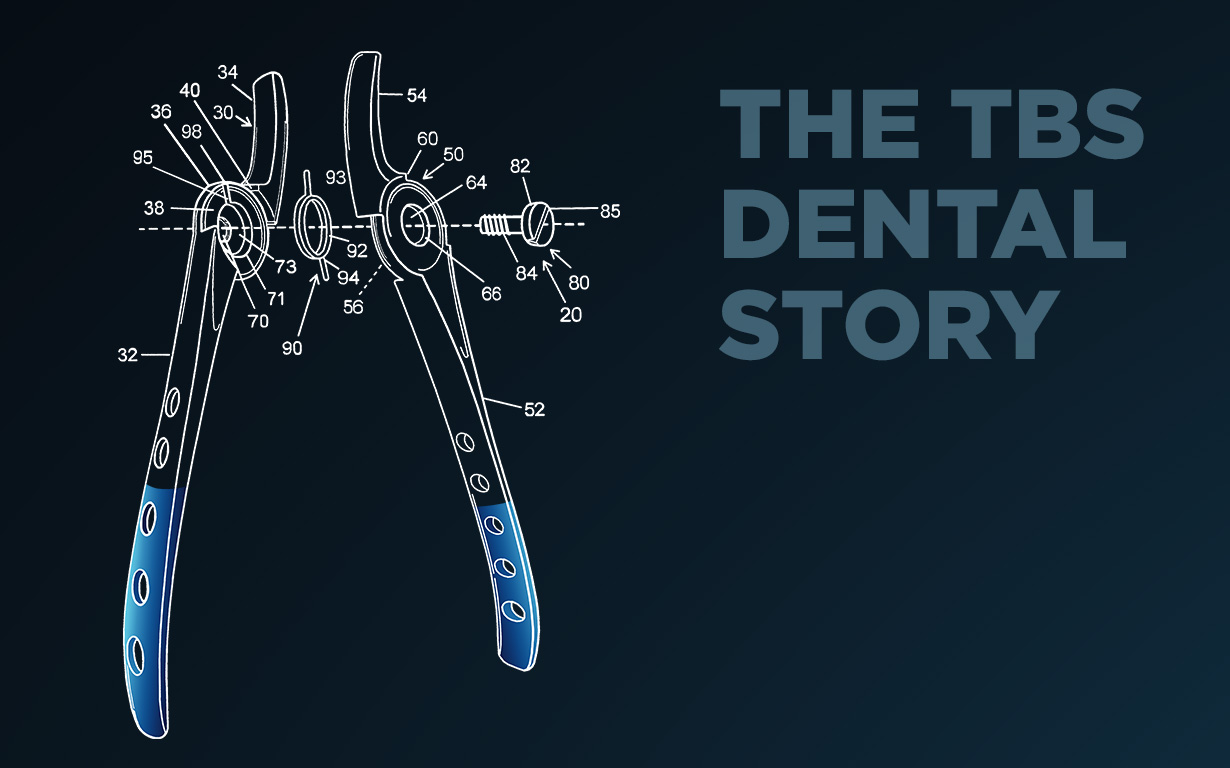
Today, with advances in segmentation software, we can virtually extract teeth and calculate the volume of graft material needed before we pick up a forceps or touch the scalpel to the patient. We can assess bone quality, anatomical proximity to vital structures, and implant trajectory to provide the link to the restoration. In short: we’re no longer guessing. That’s not surgery, that’s gambling.
And yet, I still see implants floating outside bone envelopes on social media posts. We are the engineers and architects of the oral cavity and we need a plan, we need a blueprint for success.
Bone doesn’t grow into a vacuum. We need:
Whether you’re planning to place an implant or simply preserve ridge volume for a pontic site, your grafting strategy must be intentional. This isn’t about “filling holes.” It’s about building predictable outcomes.
The gold standard is autogenous bone, but most patients don’t want a second surgical site to collect the amount of bone required. So I rely on mineralized cortical–cancellous allograft, which offers:
I’ve been using this type of bone for over 25 years. And yes, it’s from a bottle, from a highly validated tissue bank from human donors who’ve made an extraordinary contribution to healthcare. That matters.
As for synthetics and xenografts? They have their place, but many never fully integrate and can complicate future implant site preparation. My advice: stick with what heals predictably.
Too many clinicians underestimate the value of delivery systems. TBS’s curved syringes, for example, allow me to deliver hydrated graft directly into the socket with control and precision no contamination, no spill, no waste. It’s elegant and efficient.
And particle size matters. Large particles don’t work in small sockets. Match the material to the morphology; again, segmentation helps understand the three dimensional volume needed to properly fill a defect.
If you place a graft without a membrane, you’re inviting soft tissue invasion. I use non crosslinked collagen membranes, specifically from porcine pericardium. These offer:
For complex multiple implant sites, I find it useful to punch a hole in the membrane and drop it over a multi-unit abutment or for major grafting I might need to use a tack to hold the membrane in place or deep horizontal mattress sutures which is my go-to protocol. Sometimes I use the ice cream cone technique for buccal wall defects. Either way, it’s about protecting the graft and controlling the healing environment.
Surgical success isn’t just about biologics, it’s about ergonomics. I’m proud to have partnered with TBS to develop instruments like the GANZ FRINGS® – forceps with precision-aligned beaks designed for root tip retrieval with their excellent ability to grab with the innovative flat to-flat beaks. They’re not just instruments. They’re solutions for those 4:30 p.m. nightmares.
Invest in instruments that reduce fatigue, increase control, and help you do better work.
My patients aren’t coming to me for implants, they’re coming for teeth. And to give them that, we need bone. When there may not be enough bone volume, we need a plan to recreate lost volume. And to have a plan, we need adequate 3D imaging, training, and the right materials.
Socket preservation isn’t just a clinical protocol, it’s a commitment to doing the right thing the first time. With digital tools, better graft materials, and biologically sound techniques, we can deliver surgical outcomes that are functional, esthetic, and built to last.
And we can do it every single day.